Cancer: Radiation Oncology
The Radiation Oncology team use various forms of radiation to safely and effectively treat cancer, control the growth of the cancer or to relieve symptoms, such as pain. We understand the importance of research in discovering, designing and testing new treatments, and are actively involved in multiple clinical trials and research projects.
Research Areas
The EXPERT Phase III Trial (breast cancer)
Phase III studies are done to study the efficacy (that is, whether it works as intended) of a promising intervention in very large groups of trial participants by comparing the intervention to other standard or experimental care methods, and to collect information that will allow the intervention to be used safely.
Together with Peter MacCallum Cancer Centre, St Vincent’s Hospital, Western Health, Box Hill Hospital, Olivia Newton-John Cancer Wellness & Research Centre, we are recruiting people to participate in the EXPERT Trial, a phase III trial that is examining personalised radiation therapy for low-risk early breast cancer.
Radiation therapy (RT) after breast-conserving surgery is the current standard of care for patients with early breast cancer. However, breast cancer is a variable disease, which means the benefit of RT in preventing the cancer from returning to the area also varies between individual patients.
A priority in breast cancer management is to identify patients who are unlikely to benefit from RT, to avoid the associated side effects and over-treatment costs. A recent analysis of tumour specimens from over 1000 patients with early breast cancer has shown a link between the genes expressed in the tumours and the risk of the cancer returning to the area. This trial presents a unique opportunity to use gene expression to identify low-risk patients for whom RT after breast-conserving surgery can be safely omitted.
For more information visit the Barwon Health Clinical Trials site
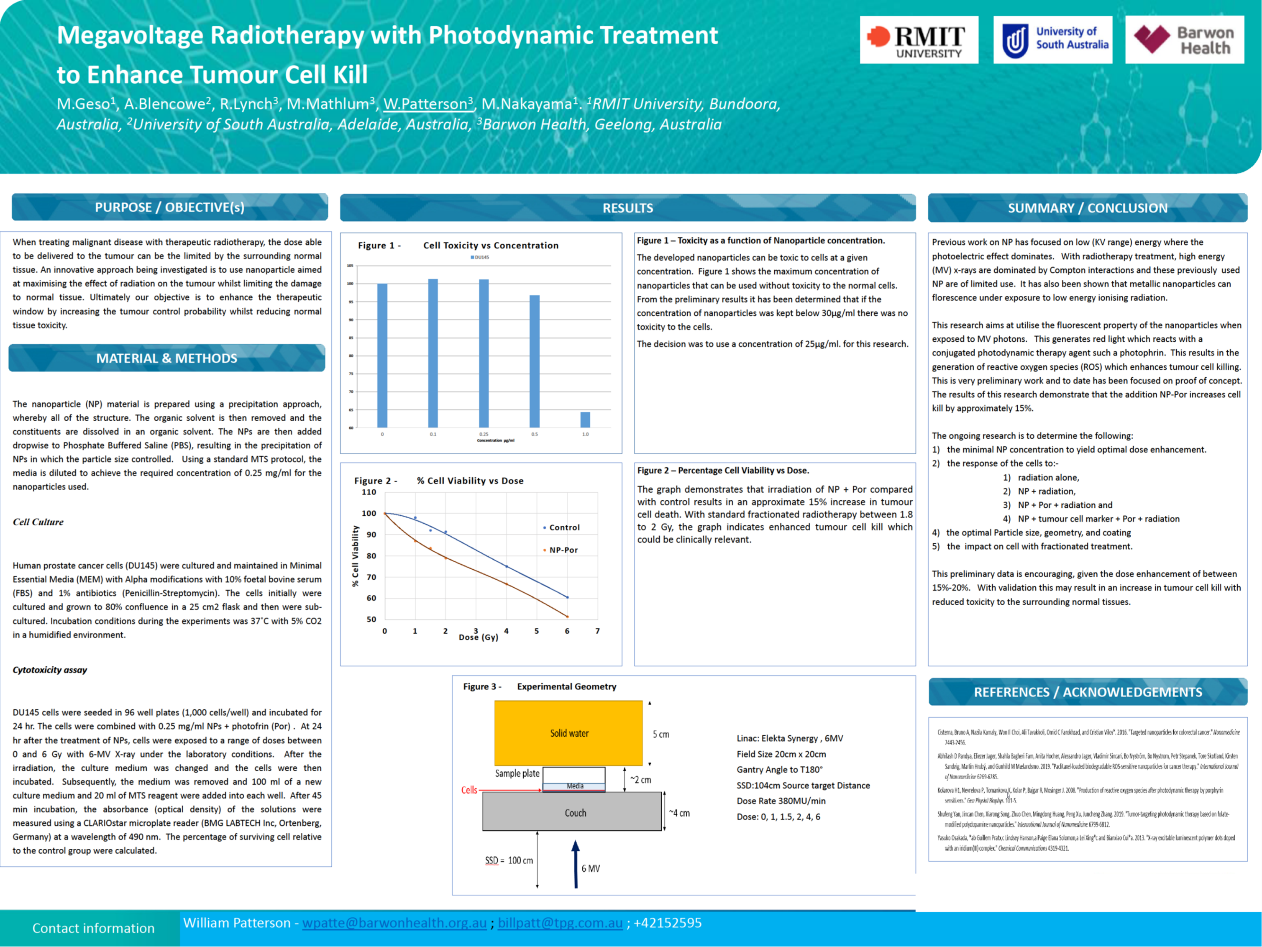
Use of a Novel Metallic Nanoparticle1 as a Radiation Dose Enhancer
A novel nanoparticle agent showing promising enhanced tumour cell kill properties is being investigated in the laboratory. Dose enhancement is achieved by the generation of more oxygen in the vicinity of the tumour which assists in cell kill. The generation of this oxygen is achieved through interactions of the fluorescent photons (produced by irradiating the nanoparticles with photon radiation) and an agent such as photophrin. If proven to be viable, this nanoparticle agent can be introduced to the tumour prior to radiotherapy to increase the dose to these cells and so increase the efficacy of treatments.
This project is a collaboration between the University of South Australia, Royal Melbourne Institute of Technology, and Barwon Health (Radiation Oncology). Seed funding has been sourced for three years to demonstrate proof of concept.
1Details of the nanoparticle have been omitted to preserve intellectual property.
Use of Data Mining and Machine Learning to Assist in Radiotherapy Clinical Decision Making
Radiotherapy is an established treatment technique with guidelines based on historical clinical evidence. Globally, there is a vast amount of data available which can be computed and processed by data mining and machine learning to assist the clinicians in their decision-making.
Radiation Oncology has ethics approval to be involved with OzCat (The Australian Computer Assisted Theragnostics network) and the global consortium to mine clinical data to produce treatment information, such as the probability of toxicity and outcome based on a patient’s clinical profile, to assist in clinical decision making.
Collaborating Organisations
| St Vincent’s Hospital | Western Health | Box Hill Hospital | |
|
Liverpool and Macarthur Cancer Institutes and Ingham Institute |
Research Team
Medical Physics
Thu Tran, Research Contact
Radiation Oncology
Dr Graeme Pitson, Appointment in progress
Radiation Therapy
Ken Wan, Research Contact
Philip Moloney
Tom Ffrench
Research News
Conference presentations by the Radiation Oncology Researchers
- Flavio Enrico Nelli: Simplified dosimetric characterization of 3D printed bolus material for electron beam radiation therapy. Engineering and Physical Sciences in Medicine Conference 2023
- Trang Pham: Shifted paradigm on linear accelerator jaw calibration: The TPS standard. Engineering and Physical Sciences in Medicine Conference 2023
- Jeffrey Harwood: Determination of representative reference and tolerance values for planar kV image quality for TrueBeams. Engineering and Physical Sciences in Medicine Conference 2022
- Flavio Enrico Nelli: What is wrong with Eclipse’s Dosimetric Leaf Gap parameter? Engineering and Physical Sciences in Medicine Conference 2020
Research in Focus: Ensuring accurate reference doses in radiation therapy
Radiation therapy uses a controlled dose of radiation to kill cancer cells, or damage them so they cannot grow, multiply or spread. The therapy is targeted to ensure that the cancer cells receive the full dose of radiation, while as little radiation as possible reaches the normal body tissue near the cancer.
For specialists to know they are delivering the correct clinical dose of radiation to the correct site in the body, it is vital that they first calibrate the radiation against a standard reference dose. Calculation of a reference dose is performed under strict conditions set by international codes of practice, however there may be specific limitations in different reference systems that users must take into account when calibrating doses.
This research, conducted by Sadia Aftab of Barwon Health at Calvary Mater Hospital, set out to test the impact of a metal rail found in the SNC 3D scanner water tank reference system, on the delivery of a reference dose of radiation.
By setting up an experimental system and varying factors such as radiation type and the location of the metal rail, the researchers found that:
For low energy radiation, which tends to be used to treat superficial cancers, the metal rail did obstruct the dose of radiation in some conditions.
This effect was not observed when high energy radiation, which is used to treat cancers deeper within the body, was tested.
These results provide a warning that in some cases, adjustments need to be considered to the reference dose calculation to ensure that the correct clinical dose of low energy radiation is delivered to the patient. Findings such as these are vital contributors to the safe and effective delivery of radiation therapy.
Featured Publications
|
Shared vision for a state-wide patient data exchange solution. Thompson, K. ASMIRT-NZIMRT 2020 Conference [Postponed until 2021]. Conference Abstract. |
|
The effect of the horizontal metallic drive on reference dosimetry in the SNC 3D scanner water tank. Aftab S, Barnes MP, Doebrich M, Lehmann J. J Appl Clin Med Phys. 2020; 21(4):95-101. |
|
Development of a multicentre automated model to reduce planning variability in radiotherapy of prostate cancer. Panettieri, V., Ball, D., Chapman, A., Cristofaro, N., Gawthrop, J., Griffin, P., Herath, S., Hoyle, S., Jukes, L., Kron, T., Markham, C., Marr, L., Moloney, P., Nelli, F., Ramachandran, P., Smith, A. and Hornby, C.J. Physics and Imaging in Radiation Oncology. 2019 11: 34–40. |
|
A Model-based Algorithm to correct for the loss of Backscatter in Superficial X-ray Radiation Therapy. [NOTE - Full text for Barwon Health staff; public can view abstract]. Harwood, JR., Nelli, FE. Physica Medica. 2019, 65: 157-166. |
|
Design and Synthesis of an Organic Nanostructure to Combine Adjuvant Radiotherapy with Photodynamic Treatment to Enhance Radiation Effects. Geso, M., Blencowe, A., Lynch, R., Mathlum, M., Patterson, W. In: Proceedings of the Amercian Society for Radiation Oncology 61st Annual Meeting, Chicago IL, USA, 15 – 18 September 2019. Conference Abstract. |
|
PSMA‐PET‐ seeing what others can't. Bowe S, Glenn C. 12th Annual Scientific Meeting of Medical Imaging and Radiation Therapy, Perth, Australia, 24-26 March 2017. Conference Abstract. |
|
VMAT-FFF Lung-SBRT QA: A Method for Routinely Assessing the Dosimetric Impact of the Interplay Effect. Nelli, F., Harwood, J. In: Engineering and Physics Science in Medicine, Sydney Australia, 2016. Conference Abstract. |
|
VMAT 5 years on ‐ the Geelong experience. Chandler S, Bowe S. InL 11th Annual Scientific Meeting of Medical Imaging and Radiation Therapy, Brisbane, Australia, 22‐24 April 2016. Conference Abstract. |
|
SBRT for Medically Inoperable Lung Cancer Using VMAT with FFF Beams: Early Experience at the Andrew Love Cancer Centre. Hui AC, Francis MP, Chandler S, Nelli FE, Pitson G. Australian Lung Cancer Conference [Details Unknown]. Conference Abstract. |
|
Impact of Altered Radiotherapy Fractionation Schedules on Acute Skin Toxicity in Breast Cancer. Nguyen K, Pitson G, French T. Clinical Oncology Society of Australia Conference [Details Unknown]. Conference Abstract. |
Support Our Research
Participate in a Clinical Trial
To find out about clinical trials currently underway at Barwon Health, click here.
Donate
Clinical trials require ongoing investment and there are several ways to support this amazing work.
You can make a donation today and contribute to an item on our research wish list, consider a bequest in your will, or establish a lasting legacy fund in your name. No matter what size, your philanthropic support with deliver an immediate impact.
To donate now or for more information and further discuss your support, please contact the Barwon Health Foundation.
Wish List
$25,000 will fund a Research Assistant to conduct a project that uses data to help decision- making for oncology patients. The aim is to more accurately predict potential outcomes of treatment in terms of factors such as life expectancy and quality of life, so the patient can make a more informed decision.
Last Modified: Friday, 22 September 2023
Research Contacts

Dr Graham Pitson, MBBS, FRANZCR
Appointment in Progress
Ken Wan BSc RT, MSc RT , MBA
Chief Radiation Therapist

Thu Tran, BSc (Hons), MAppSc, EMBA
Chief Medical Physicist
Related Links